By JP Leider, PhD, Center for Public Health Systems, University of Minnesota School of Public Health and Laura Power, MD, MPH, Preventive Medicine Residency and Office of Public Health Practice, University of Michigan School of Public Health, Region V Public Health Training Center, Public Health Prepared
Last week was the Michigan Premier Public Health conference, held in the scenic Shanty Creek Resort in northern Michigan. Imagine fall colors on water. It beats, by a long shot, concrete conference centers that we all might be used to. More than that though, with over 400 local and state public health practitioners coming together wanting to talk about their field, their practice, it was energizing. We talked about the state of the science, programs and evaluation, some of the work that everyone is doing. The issues we are facing. Seems those issues are many and varied.
As part of the Center for Public Health Systems work, I (JP) was lucky enough to be able to kick off the event, and as part of the Region V Public Health Training Center, my team (Laura) presented on a number of issues related to the training needs facing Michigan public health practitioners. What follows are some highlights.
Greater participation means greater insight
Thoughts from JP
As we have talked about on this blog before, the Public Health Workforce Interests and Needs Survey is one of the best data sets for understanding individual public health practitioner perspectives on job satisfaction, employee engagement, intent to leave, and demographics, among other items. Over the past 10 years, PH WINS has evolved and become a mainstay in the public health research community. One of the big changes in 2021 was the PH WINS for All pilot, where in Regions 5 and 10, small local health departments were invited to participate alongside other midsize and larger locals. This resulted in far more health departments participating, meaning more responses overall and giving researchers, health agency officials, and the field itself a deeper insight into what makes practitioners tick. At all levels. In Michigan, especially, this is true, going from 300+ respondents in 2017 to 1,300+ respondents at the state and local levels in 2021 – we know a lot more about Michigan public health staff interest in training needs and intention to leave, among other key indicators. It is only with the participation of these health departments and their staff that this insight is possible. Agencies also get dashboards particular to their own organization for participating (and hitting needed response rates).
Figure: PH WINS Participation in 2017 and 2021 in Region V
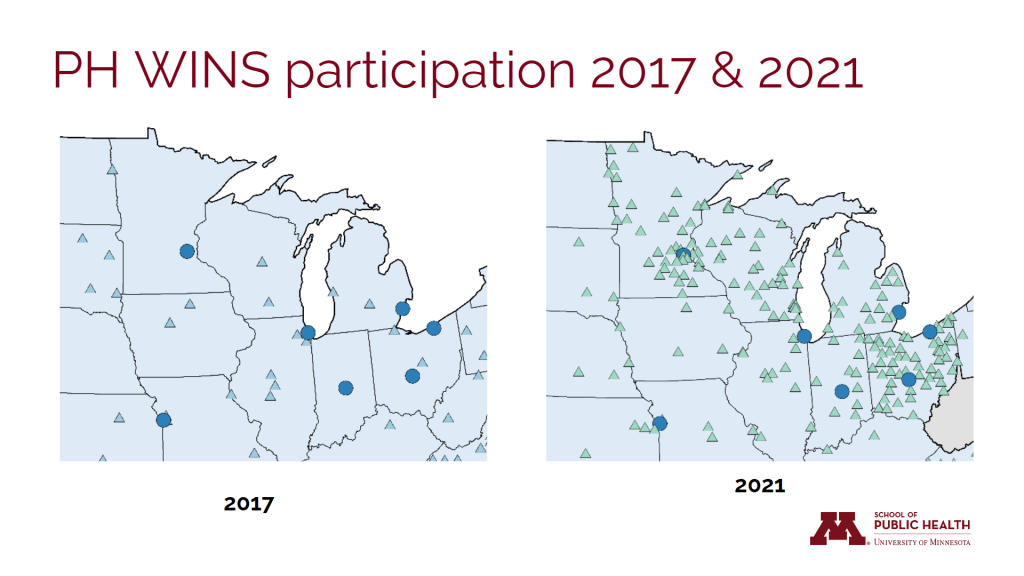
Source: de Beaumont Foundation
When the MPPC kicked off, the organizers shared a sobering statistic: at least 40% of their workforce had turned over in recent years. That fairly closely matches data out of PH WINS showing that approximately 40% of the workforce in Michigan, as nationally, has worked less than 5 years in public health. This is a stark departure from the past, and follows a trend of decreasing tenure in one’s job, and one’s organization, at all levels, including among top executives.
On the one hand, it is depressing to see such turnover, that people join and don’t stay. On the other, it is not particular to public health – it’s not the Great Renegotiation (in public health), or the Great Reshuffling (in public health). This is sector-wide, industry-wide, generation-wide. There are things that are affecting public health a little bit more that relate to pandemic and public sector response. It is true that we do not pay as well as our most stringent competitor, the health care sector. Nobody does really, other than tech. We are between a rock and a hard place there, and can’t and don’t compete on paid with those two sectors.
Figure: Agency size by tenure in public health practice
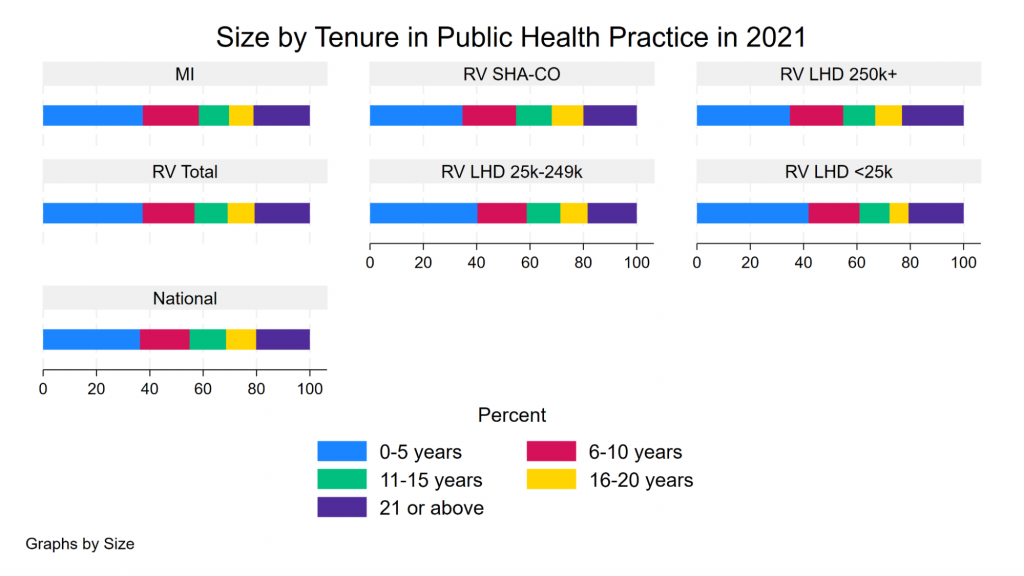
Source: de Beaumont Foundation. Note: MI – Michigan. RV – Region V (Illinois, Indiana, Ohio, Michigan, Minnesota, Wisconsin), LHD – Local Health Department, SHA-CO – State Health Agency-Central Office, numbers indicate size of populations served.
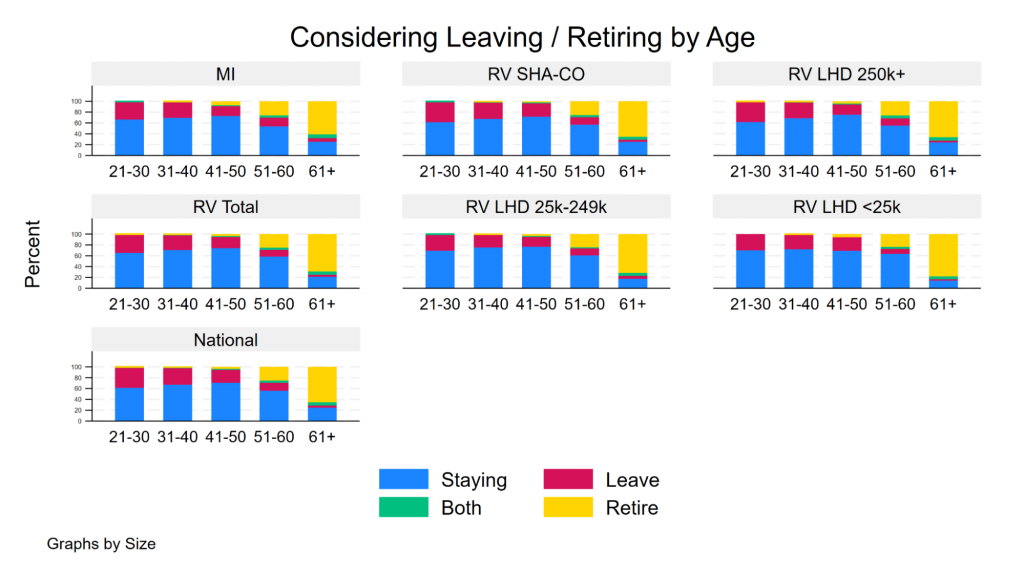
Not all staff that consider leaving do so, but the proportion is substantial (35%-50% in recent years). So it is similarly substantially concerning that even despite all of that turnover, a pretty big chunk of the workforce is still thinking about leaving. Some are thinking about doing so through retirement, but a bunch are thinking about just plain quitting. And that turn over intention is substantial for people under the age of 35. But, there are some bright spots – despite relatively high turnover intention, there remains high levels of job satisfaction and pay satisfaction, as true in Michigan as it is regionally and nationally. A little perplexing at times, but true.
Figure: Considering leaving/retiring by age in Region V
Highlights from the RVPHTC
Thoughts from Laura
I could feel the warmth of those bright spots at the conference, just like the sun coming through the colorful northern Michigan trees. But more than the scenic setting, it was the energy of people coming together with the purpose of improving public health that felt bright and hopeful. And, in the spirit of the conference theme – Reconnect and Reimagine Together: Building the Public Health Workforce of the Future – I was energized by the people around me. Despite the turnover in our public health workforce, I saw many familiar faces of people who have been serving Michigan’s public health for years alongside newcomers to the field. Together we reflected on the workforce, connecting our individual experiences with the trends that JP eloquently described in his opening keynote presentation. It was a helpful reminder that the turnover we are seeing is not unique to public health and that the workforce overall is shifting.
Still, there are unique challenges and one that I still grapple with is how to acknowledge the trauma experienced by public health workers while also promoting governmental public health to students and trainees. Some of my colleagues at this conference have experienced threats, trauma, backlash, and yet they are here reimaging and energizing the rebuild of the public health workforce. I’m amazed at the resilience of my colleagues. People care about public health. I like that the conference encouraged us to reimagine the concept of workforce development – as described by Joanne Pearsol, Director, Workforce, Association of State and Territorial Health Officials and the 2nd keynote speaker of the conference, workforce development more and more is referring to things like well-being, belonging, and balance.
With huge numbers of undergraduate students choosing public health as their field of study, soon they will be looking for jobs in public health. While we think about how public health jobs can be more appealing to these soon-to-be graduates, we must also think about that multifaceted approach to workforce development. We need to prepare for a workforce that is more fluid and we need embedded training, development and support. And it all comes back to the data and knowing about the workforce. (Please participate in those needs assessments and keep a look out for the next fielding of PH WINS!)
To learn more, check out these resources:
- Using PH WINS Data to Enhance Your Workforce Development Planning (Self Paced-No CE)
- P2P Workforce Development Series (Program-No CE)
- What Can the State of Michigan Tell Us About the State of the Public Health Workforce? – JPHMP Direct

